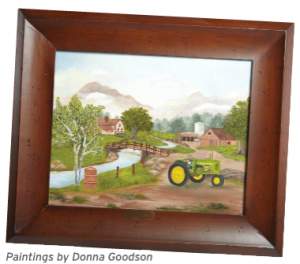
Former D4C Board Member Donna Goodson
Time, trust, and Texas Health Resources’ commitment to collaborative medicine helped give a Euless woman her life back.
For years, Donna Goodson, 66, experienced a cascade of bad luck: the deaths of her parents, stomach and back trouble, a broken leg, and a torn hamstring. Given that history, she wasn’t able to eat right or move around as much as she wanted, so she spent many of her recent years lying on her sofa in pain. When she began experiencing sharp discomfort in her chest, Donna attributed it to anxiety about the emotional and physical distress she’d been suffering already. Luckily, Donna’s primary care provider, Marc Chapman, M.D. internal medicine physician on the medical staff of Texas Health Harris Methodist Hospital Hurst-Euless-Bedford, took her complaints seriously.
“I was having twinges of chest pain and breathlessness. I thought it was stress,” Donna says, “Dr. Chapman didn’t agree.”
 Dr. Chapman referred Donna to Neeraj Badhey, M.D., F.A.C.C., C.D.N.C., S.C.C.T., an interventional cardiologist on the medical staff at Texas Health Hurst-Euless-Bedford.
Dr. Chapman referred Donna to Neeraj Badhey, M.D., F.A.C.C., C.D.N.C., S.C.C.T., an interventional cardiologist on the medical staff at Texas Health Hurst-Euless-Bedford.
INTERVENTION, JUST IN TIME
“I first met Donna in May 2012,” Dr. Badhey says, “She was having chest pain that limited her lifestyle significantly. In fact, she couldn’t even do laundry.”
Favoring a conservative approach, Dr. Badhey ordered a stress test and prescribed anti-angina medications for Donna. However, within just two weeks, Donna experienced increased chest pains, visited the Emergency Department, and was prescribed more medications.
Despite her medications, Donna’s chest pain was still limiting her activities drastically. In these cases, Dr. Badhey says, cardiologists consider angiograms and stenting.
“At that point, we performed a coronary angiogram and found that Donna had 85 to 90 percent blockage in one artery,” Dr. Badhey says, “Situation was a little complex based on her anatomy, but in consultation with her family, we decided on a stenting procedure, and I carefully placed a stent.”
In fact, the stenting procedure can be quite variable, depending on patient anatomy and the location of the blockage, Dr. Badhey says.
“The procedure can take an hour and a half to five hours,” he explains. “No two people are the same. When people have multiple blockages, they may be candidates for bypass surgery, whereas people with a single blockage are often amenable to stents and can go home the next day.”
“Donna had a single blockage, but it was at the intersection of two major blood vessels,” Dr. Bradhey says, “It was challenging because I had to place the stent correctly within one to two millimeters.”
SUCCESS, SLOWLY BUT SURELY
Donna’s stenting procedure was a success, but for a while, she continued to experience chest pain. She tried cardiac rehabilitation, but the trials she had experienced during the past years were weighing her down. Heart disease seemed like the last straw.
“When they told me I was a heart patient, I burst into tears,” Donna says. “I didn’t believe it. I was living in fear.”
Eventually, encouraged by Dr. Neeraj and her therapists, Donna embraced cardiac rehab with a renewed spirit.
“My therapists treated me with such respect and expressed so much compassion for me,” Donna says, “they would come up and pat me and tell me how proud they were. They never tried to force me. Gradually, I could see my progress. Now I walk for an hour, five days a week. I’ve become active in my church and can even serve as church treasurer again.”
A LIFE RENEWED
Once, Donna refused to believe she had a coronary blockage. She cried when she thought about what was happening to her. But, as she grew stronger. Donna developed a new mission: educating other women about heart disease.
“I’m participating in Women’s Heart Week,” she says, “I want to encourage women to take care of themselves and learn from my experience. I believe God gives us stepping stones in our lives. Coming to terms with my heart disease was a major stepping stone for me. Women need to take heart disease seriously, and also to know that there’s hope.”
RISK FACTORS
Like Donna Goods, no one wants to believe he or she has heart disease. But if you have any of these risk factors, you should take the possibility seriously and have a talk with your primary care provider about steps you can take to reduce your risk.
• Diabetes and prediabetes
• Family history of heart disease
• High blood pressure
• High cholesterol levels
• Not being active
• Overweight and obesity
• Poor diet
• Smoking
• Stress
To read the Texas Health Article click here and turn to page 6.